Research lives and cultures
Research lives and cultures
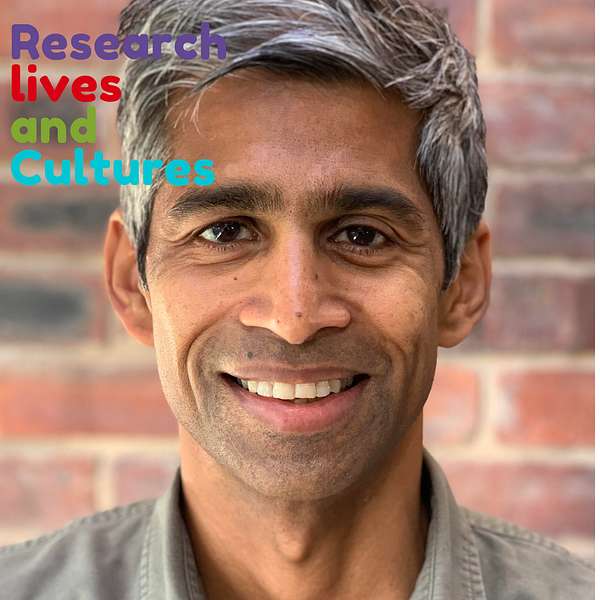
60- Prof. Thushan de Silva- When building compartiments between clinical and research practice creates better focus
Prof. Thushan de Silva is an Infectious Diseases Clinician Scientist at The University of Sheffield.
His research journey started during his medical training and continued thanks to several clinical fellowships that have allowed him protected time to build his research portfolio alongside continuing clinical work.
Thushan is currently working as a Senior Clinical Lecturer at The University of Sheffield. He was heavily involved in SARS-CoV-2 research through the COVID-19 pandemic and was recognised with an MBE in 2021 for services to COVID-19 research.
It took Thushan several attempts to obtain a funded Clinical PhD but this did not deter him from following a mentor to undertake a PhD at an MRC centre in the Gambia. This was the perfect hub for a clinician interested in infectious diseases to experience both field work and laboratory research.
This extended period of research in the Gambia during an MRC Clinical Research Training Fellowship and a Wellcome Trust Intermediate Clinical Fellowship provided a fertile terrain to build his research portfolio, but also to understand the culture of undertaking research in a Global South context. This gave him the time to build a strong network of colleagues and collaborators committed to undertake work in the African context.
Researchers often worry about changing research topics at the end of their PhD or Postdoc. Thushan did change his research direction and accepts that it can be difficult to articulate a congruent and powerful narrative about a shift in research direction to the funders. His logic of choice came from feeling more inspired to continue his work on vaccine development instead of remaining in the area of pathogenesis of HIV-2 infection and the molecular epidemiology of HIV-1 and HIV-2 in West Africa.
Identifying the right balance for compartimentalising research and clinical practice is a crucial step for Clinical academics. It is likely that it will require substantial negotiations in the clinical setting and the academic department.
It may be worth encouraging new clinical academics and clinical PhD students to explore what is working and not working for them. They may not know until they have started. Getting them to become aware of what is going to be manageable in the long term is essential. If a pattern of clinical and academic work has been set but is not working, or is just not manageable, encouraging clinical PGR or clinical academics to not give themselves such a hard time, but go back to the drawing board and explore alternative options for work patterns.
Listening to our conversation will prompt your thinking:
- Are the boundaries between your research and clinical responsibilities working for you?
- Are the boundaries between your research and clinical responsibilities working for you, or are you trying to be a superhuman?
- Could you negotiate an alternative pattern of work that would allow you to be more focused and effective in both area of research and clinical practice?
- How are your clinical and academic environments supporting and valuing your dual career?
- What additional research skills could you consider gaining early on in your clinical research life?
All right. Let's get started. Good morning. Good afternoon. Good evening. Dear listeners, you're on the podcast, research lives and culture. And today I have an academic. With a little bit of a different type of academic, I suppose, is a clinical academic. So I have with me today Professor Tushan De Silva. Welcome on the show.
Thushan:Thank you very much for having me on.
Sandrine:So it will be really interesting to hear about your career. So in the last few months, I've been having interviews with people who are like you, doctors, but who also have the craziness. of doing research. And I'm really fascinated by the, the courage that it takes to have this dual career. There are lots of, lots of people in medical professions who are interested in, in research and are attempting to combine their clinical practice with research. And it's, it's difficult. So it would be really fascinating to hear how you've got there.
Thushan:Yeah, sure. I mean, I, I mean, I, I guess the first thing before I, I do that to say is I, I, you did say it's sort of, you know, crazy to do both, but it, it is a real privilege, and maybe we'll get onto this a bit later, about just how enjoyable it is to, to do both. So I I'm an infectious disease clinician scientist, so my sort of clinical speciality is infectious diseases. I didn't always want to do that. And in fact, my first experiences of research were at medical school. When I did what's called an intercalated. BSC. So you spend the third year of medical school away from medicine doing a research project. And at the time I was very interested in psychology and neuropsychiatry. So I did a psychology BSC and I did a project around looking at Cognitive processing to see whether you processed information subliminally. And this was really my first experience of, I guess, experimental design which I enjoyed very much. But then I went back to medicine and I developed a passion for infectious diseases. And my kind of next experience of research was Trying to apply for funding to do a PhD and that was actually an eye opener very early on because I think I applied for five different fellowships before I was finally awarded one by the Medical Research Council. So that was quite an early. Lesson in, I guess both resilience in academia challenges with funding and also I guess what's required to kind of write successful research fellowships.
Sandrine:So some of the choices that, that we have to make in research is to actually decide on a research topic. Especially when you're trying to get funding, you may have an idea of what you want to work on, and you may not be able to, especially very early on, you know, when you want to do a PhD, so how did you decide what you wanted to work on? And how did you decide to do it? was it a matter of repeating multiple times, with the same sort of topic, or did you have to change, you know, really drastically to the type of research that you apply to do for your PhD?
Thushan:it was variations on a theme that I applied for, so I didn't change drastically between application. I guess in terms of choosing the topic I'd say sort of clinical infectious diseases and training is, is. probably one of the more academic, you know, specialities. And so at the time when I was at the right point in thinking about doing a PhD during clinical training, I was doing clinical work in Oxford and there's quite a, I guess, vibrant infectious disease, you know, research portfolio. So. I went and spoke to a variety of people just to talk about the different projects and areas that I could be involved with. And came across, I guess, at the time, what I thought was, the right mentor to kind of guide me as Professor Sarah Olin Jones. And she was at the time taking up a position at the MRC unit in the Gambia as a director of research. And the area of research that she was working on, which was kind of looking at the differences between HIV 2 and HIV 1, and, and why one behaved very differently to the other really intrigued me. And I guess the combination of kind of field studies. And linking them to laboratory science really excited me, I guess I didn't really quite realize that at the time, but that's really where my sort of passion lies and where my skill set is. And that's kind of continued through my career,
Sandrine:So did you then do partially your PhD in The Gambia or?
Thushan:Almost entirely. Quite a bit of my kind of research career until recently. I was based at the MRC units in the Gambia. So both of my PhD sort of training fellowship as well as then my career development fellowship. I went back there. So I probably spent about 6 or 7 years full time based there. But each fellowship with a period of time in UK laboratories as well.
Sandrine:So how do you feel that you have sort of transitioned? Because when you choose a topic for your PhD, you work with a supervisor, but then applying for, the various fellowships afterward, this idea of, the process of transition towards research independence in the sense of building your own research ideas, kind of trying to detach ourselves from, you know, from an academic supervisor to, to build their own projects. How was it for you?
Thushan:Yeah, it's an interesting question, and I mean, I think there are different paths to that. In my case, I really changed fields, although I think there were generic skills that I took forward to my next stage and then beyond. But I changed topics, so while I worked on HIV 2, sort of viral immunity and molecular epidemiology in my next stage, I kind of switched to vaccine immunology. And there were several reasons for that. While I was at the MRC Gambia, I was really inspired by, I guess, a lot of the vaccine immunology work that was going on. And it felt like an area that not only was, you know, incredibly exciting and interesting, but but you could also have an impact you know, in terms of the work that you were doing and I moved, institutes, as well, so I I Came back to Sheffield to finish clinical training. And, you know, had other mentors that I got help from as well. So, all these things together kind of led me to The decision of, you know, applying to, to do a very different topic and, and one which I then thought I would want to take forward in the rest of my career. So that's how I approached it. There were challenges with that, clearly, you know, articulating why you've changed to a kind of funding body. Needs to be done in a, in a thoughtful way and in a coherent way which you know, thankfully I think I managed to it's obviously easier to build a narrative around your applications if you have stayed within the same field, but as you've highlighted it, then Comes with the challenge of trying to find your own niche and showing your independence. And clearly there are ways of doing that.
Sandrine:So what made you decide to change?
Thushan:What made me decide to change fields think it's. largely because I found the field of, vaccine immunology you know, incredibly exciting and interesting. And, you know, while my PhD gave me lots of, you know, generic skills in the lab analytically and also running sort of field studies you know, gave me a good springboard and a platform for going forward. I, I didn't feel that that topic was something that I, I, Could or wanted to spend the rest of my career doing. And you know, interestingly, so after my PhD Viva you know, one of my examiners said, well, I, I don't think there's really room for two groups in the UK working on HIV too. So, you know, you probably want to think about something else. that, that was also, I guess, a piece of advice that made me really think that I, I should change.
Sandrine:So somebody protecting their territory probably as well.
Thushan:Well, no, I mean, to be fair that that wasn't you know that, that was an external examiner, not my supervisor. In fact, my my supervisor is a, is a colleague now. And she often that was try and keep me interested in HIV two and asked, so I, I don't think there was any sort of. territorial protection. But, you know, I think we have to be realistic in terms of the funding climate that we're in. So I think that was just advised from a, from a very wise, senior academic about thinking of where you want to position yourself you don't want to. be in competition to, I guess, close colleagues and, and I guess my supervisor at the time.
Sandrine:So when you were doing your PhD and after your first fellowship, what was the balance of your clinical practice? So where are you still working in the clinic in the Gambia
Thushan:So during my PhD, I mean, because I was, you know, 100 percent funded by the, the Medical Research Council on a fellowship, you know, there wasn't any requirements to do clinical work. But as, as with many clinical academics listening, especially in infectious disease academics, if you're working overseas, you're interested in, you know, still doing some clinical work and as with others, you have anxieties about losing some clinical skills. So, I, I sort of did a small amount. So, I did, I think, a clinic either once a week or once every two weeks while I was in the Gambia. And then when I returned, I had a period of full time clinical. training for about a year, year and a half. And then I was very fortunate to get an academic clinical lecturer post, which is part of the kind of Walport scheme. It's a way essentially, then you have 50, 50 percent time dedicated to clinical work and 50 percent to research. And in that research time, they're really designed to try and allow you some space to generate ideas. Generate networks and generate preliminary data to write a fellowship application for your next stage. So, yeah, I probably did that for about three years, I think, the 50 50. And during that time, I sort of finished my higher specialist training in clinical infectious disease and medical microbiology.
Sandrine:When you work in an academic setting, people work very long hours, even though there are so many conversation about, you know research culture and having balance, the, the reality on the ground, for people to actually get the funding and get the data and so on, it's, it's, it's very challenging. So. What is it like to actually be, you know, a academic and still having, you know, the clinical role?
Thushan:So I mean obviously, and others will tell you this, it, it's, you know, the, the, the two halves of your job don't add up to a hundred percent. Right. And, but that's, you know, true of many people who have dual roles, not just clinical academics. So that, that's a big challenge because I think either side, so to speak. Doesn't see the full picture of what you have to deliver for your other master. And I think on the, on the clinical side, job, job planning. So actually working out what you do with each. bit of your day is a lot more defined. On the university side, that's very ill defined, and that's partly because it's quite hard to do. So I, I would say that on both sides, there are just lots and lots of hidden, in inverted commas Demands on your time. And you know, that that just means that you are, you know, you're functioning at at least 150 percent if not more. So that that is a challenge to try and get the balance, right? And clearly, then, you know, trying to get right with then, you know, your home life as well.
Sandrine:so what do you think that you've done well? In creating a balance for yourself what do you think over the years you've really worked really hard at doing in terms of maintaining your wellbeing, you know, maintaining your sense of, you know, not, not losing the plot because of all the demands that are on your time.
Thushan:There's quite a lot to unpack there, I guess. I mean, the first thing to say is that I, I think, and you know, my supervisor, my PhD supervisor said this to me, if you can actually get externally funded fellowships I mean, that it's not a route for everyone. And there are many ways to do research and science, but That really does protect your time. And I think that I've really benefited from that. So as you said, you know, three years of PhD fellowship from the MRC, and then it was a five year fellowship from the Wellcome Trust as a career development and the Wellcome Trust, they stipulate that you shouldn't spend more than 20 percent of your time doing clinical work. And I think, especially at that point, Very crucial stage of your academic career development. Having that space for research is really important. So I, I really benefited from that, you know, I've had a different experience than some people, but that I just want to say that, that that's. Probably been the biggest, most important factor in me managing to kind of you know, maintain that balance. And then equally, when I first then, you know, came back to the University of Sheffield the head of department at the time, actually, she, you know, Volunteered and said, I think you need more time to dedicate to your research than our standard contracts, which are 50 50 split. So she said, I think for the first 2 years, we'd be happy for you to have a 70 30 percent research, 30 percent clinical. And again, that was just incredibly helpful because it's at a time when you're trying to. Build your team, you know, build your research area, establish your independence. So that's been crucial. And the other thing is just from the clinical perspective, you know, I work in an incredibly supportive clinical department who value you know, having academic colleagues and What I've chosen to do is, I guess, you know, I've quite compartmentalized blocks of time that I do clinical work in. when I'm on the ward, I kind of do ward work and clearly there is spillover. You know, when I kind of leave that, but it's, it's a bit easier to compartmentalize that. And so then when I'm away from the board, so that that's just something, I guess, not unique, but that I've managed to put in place. But many others do clinics every week. And I, I think I, I would find that very difficult because, you know, I think splitting your week when you've got these other demands is, is it's commonly done, but I think that's a real challenge because then everything bleeds into each other,
Sandrine:So in, in your case to be against, be quite specific so that people can hear the way that you split your time. So is there a week, are there weeks where you're completely research and then a few days where you do your clinic,
Thushan:I have, I have. Weeks you know, several weeks within the year where I'm completely sort of clinical and then other weeks where I'm completely research, although, you know, there are commitments within the week, which can be clinical as well, but they're ones that don't then demand my time outside of the allocated slot so yeah that that's been important for me and that sort of arrangement is also important because i've increasingly find myself, A way for work For research, right? So I still have lots of projects at the MRC unit in the Gambia, and we've got you know, projects in Zimbabwe, and now as I've kind of progressed, I guess, you know, time on interview panels and examining PhD thesis and things like that. So having allocated blocks where I'm on the ward, and then when I'm not, I don't need to be there is very useful.
Sandrine:I mean, it's interesting because it's, it's really compartmentalizing, you know, in the year
Thushan:yeah, I think, you know, different arrangements work for different people and, you know, the same thing doesn't work in different specialties. But I think that, this is a, maybe a nuanced point, but when you're doing clinics, outpatient clinics, there's often admin that, seeps over you know, beyond that time. There's always test results to follow up and letters that you have to then follow up and, you know, communication. And so that's very hard to compartmentalize then. Whereas, you know, blocks of time on the ward and off the ward is a bit easier to find a line. It's not perfect, but yeah, it's, it's easier to make that separation.
Sandrine:of the things that you said earlier I think is really important is the, conversation with your head of department and this person realizing that the situation for clinical academic is different and the needs are different and actually acknowledging it and doing something about it when you're setting a research group, it takes a long time to get things settled and organized and actually enabling people to have that slow burn of getting things set up instead of trying to do everything from the start is actually, really good line management, if I may say, in a way of setting people for success instead of expecting them to juggle absolutely everything from, from the start.
Thushan:Yeah, you're absolutely right. And, and, you know to go further, you know, we're not setting them up for failure, right? So, yeah, Sheila Francis, who was head of department at the time. And I, I think, you know, I, I totally just value her vision in allowing that to happen because it it helped a lot. That was really crucial.
Sandrine:When you think about the activities that you've been involved over the years, what is valued, for you as a clinician is different from what is valued, you know, for promotion, in the university context, so how have you navigated your academic career to be able to do things that again were manageable in the context of having that, that dual role?
Thushan:A good question. I mean, one thing to maybe start with which relates to some of your previous questions. I think one of the biggest problems that clinical academics face is that the demands are the same, right? So when we have annual appraisals for our clinical jobs, we have to hit exactly the same. as full time NHS you know, full time NHS doctors. And I couldn't see that the kind of promotion case for the university was really any different because I was a clinical academic. I think that the targets that I was expected to hit were exactly the same. And I think. You know, both sides could really do with a bit of thought about really what's realistic or why are we asking people to fulfill things as if they're 100 percent one or the other? Your question was how have I managed to sort of do that and balance that out? I probably made Choices in terms of the citizenship and teaching and yeah, aspects like that, other than the research on the academic side that are sort of directly aligned with some of my research interests, I guess, and, and there's some mutual benefits in me also. you know, doing that task to my research, whether it's learning for me or, you know, mentorship for others or something like that. So I think I've probably made choices that have been mutually beneficial,
Sandrine:so you've, you've been building a research group. what was your approach building your research group? You know, there's lots of academics who work part time, but obviously because you have this dual role. How has this influenced the way that you have recruited, who you've recruited in your team?
Thushan:I mean, I like to say I had a grand plan that I followed, but that would, that would be lying. So I, I think I think one thing is it's probably a mix of skills. My group consists of both clinical and nonclinical early career researchers. So I think that's probably something that isn't isn't unique to clinical academics, but more clinical academics will have that mix. And because of the sort of work that. You know, our group does. I also have a mix of wet lab scientists and analytical you know, data analytical scientists and bioinformaticians. And, and the other kind of mix is that because I have still lots of. work that is based in two African units. You know, I also have individuals, there's quite a lot of, I guess, you know, two way cross fertilization. So I've got clinical fellows who are based in the Gambia doing their PhDs and have training visits for, you know, Gambian or Zimbabwean scientists who come to my lab. So yeah, I, I guess. Variety and mix is probably how I've approached them.
Sandrine:if you're trying to, um, To sort of reflect on your journey as a clinical academic, what do you think have been key decisions, in terms of, enabling you to be where you are at now.
Thushan:There's probably too many things to mention, but let me try and, I mean, I, I think decisions about where I was based are very important. So obviously, you know, spending time as an early career researcher at the MRC units and the Gambia has had a, has a huge influence on me scientifically and, and what I do, just the sorts of work that goes on, but also in terms of You know, my passion for wanting to kind of help with scientific capacity building in those settings. And, you know, that's that's a key philosophy. I think of, you know, what work or how we do work in our group. But then also coming back to location my choice to, I guess, come back to Sheffield and the reasons for that, and a lot of that has to do with, you know, Research environment and, and, and culture and what seemed like the right thing for me, not just academically, but clinically and personally. So, I think most of the choices I've made about what I do have been driven by not just you know, where is best academically, but really where's, you know, best for what's important in my life. And, and, you know, I think Sheffield's in an incredibly collegiate environment and it's a very collaborative environment. And so I think that has been very important in me continuing to enjoy science despite the stresses. And equally then also the sort of collaborators networks that I have of many, many collaborators throughout the world. And I've always chosen to work with very nice, open and, you know, exciting, collaborative people. And those relationships are really what I think have driven, you know, how well the science has gone and how much I've enjoyed it.
Sandrine:One of the thing I'd like to ask, which in a way is less about the career, but more in terms of the context of having worked in the Gambia, because research culture, Changes, you know, from one country to another. Is the equity in the collaboration that researchers have, with researchers from the global south. And you were talking earlier about, you know research capacity building. It's interesting because I remember there was a funding scheme a few years ago where funding from the the aid budget had been given towards projects basically to develop collaboration with researchers from the global south. And then At some point, the government decided to cut the funding for that, and some of these projects were midway and couldn't carry on. So there was a lot of resentment that existed in terms of this collaboration being built slowly, and then suddenly the funding wasn't there. What do you think is really key in engaging with researchers from the global south so that there is a sense of equity and respect instead of researchers reaching out because they have to, because the funding says so.
Thushan:Yeah, so clearly there are many different scenarios and there's no one size fits all. So, I mean, I will speak from the lens of someone who does, you know, laboratory, applied laboratory work in those settings. Clearly, if you're talking about, you know, social science, for example, you know, the kind of approach will be very different or directly sort of policy impacting work. I think obviously the bottom line is that, you know, that your partners you need to consider what their, what their needs are and what they want to get out of it. And you know, the way I guess we've approached doing laboratory science um, in the Gambia and other places is trying to do as much as possible on site. Which is far more challenging than doing it here. But, you know, if, if an assay can be done on site, then we do it on site rather than take samples and do it in the UK. If there's a reason why it can't be done on site, and that's often the case, you know, there's a key bit of equipment that isn't there, or the facilities aren't quite there, then we build in. Training for local scientists so that, you know, the next grant that comes along, we can try and apply for that bit of equipment, and then we can set the essay up. And then also thinking about career development. I mean, I mean, this is obviously important, not just in, you know, low income countries, but, you know, here as well, but really thinking about Whether it's kind of higher degree support or papers or just training full stop, just putting in as much as possible for the local scientists involved in your project as something to get out of and, you know, and mentoring them. So, you know, I, I think do a lot of that, I guess, even individuals who. Haven't been to Sheffield, but you know, there's several people kind of in the Gambia that trying to mentor to the next kind of stage and help. So that's been My approach, and I think I've learned that through my own mentors. So not just Sarah, who's my PhD supervisor, but Beate Kampmann, who was my sponsor for my career development fellowship, who was based there. So it's been direct learning and I hope adopted the right approach.
Sandrine:So what advice would you give to a researcher, clinical academic who is interested in starting to collaborate, with, the MRC center or, you know, researchers, in the global south, because you had the advantage of already having spent several years, in the Gambia and building and actually understanding the, research culture, within this specific country. But if you are, an academic in the UK who has the desire to start collaborating and doesn't necessarily know where to start, what, what are the things that people should have in mind or think about, in the way they start to engage?
Thushan:So I guess the first thing is you need to find an interested and strong partner who is in country. As you said, you know, I was fortunate because I've spent time in the MRC that have many friends and colleagues there. And you need to. Work on something that is considered important in country and then have a two way dialogue about what the partner wants and find a strategy where each party can achieve their objectives and, and you're kind of stronger together. And, and that can come in many forms, right? I mean, the sorts of career development for young scientists that we talked about, it can, Come in sort of capacity building from a laboratory perspective. It can come in doing work that then directly impacts policy and more linkage with ministries of health and so on. So there are many, many forms that that can take. But I think finding that strong partners is really key. And I think finding something that works for both parties in terms of your. Actual presence there, or presence of your team members there? So I was really worried when I moved away because the kind of idea of doing remote, remote research really worried me and I about how to approach that. Because, you know, I couldn't for, you know, personal reasons be based in The Gambia anymore. So yeah, I think finding something that, that. Works for both parties in terms of, how much involvement and presence you have there is important.
Sandrine:So what's the biggest challenge that you have faced, that you are facing
Thushan:Clearly funding is a big one. I think the one thing that, you know, does keep me up at night from a funding perspective is that suddenly being responsible for other people's salaries. I think more than thinking about whether I'll have funding for my research, suddenly you increasingly become. Responsible for a group and obviously some people you can mentor to get their own fellowship funding and you hope then that they can gradually, not be your responsibility and in a nice way. But you need to kind of keep finding money. So that always feels incredibly fragile you know, thinking about. This sort of patchwork of how to keep that going. So I think that is one of the greatest challenges and I'm not sure it will really stop. And the other thing is really knowing. What to say no to and I don't really think I am very good at that, but I'm trying to be better. Especially when again linked to the funding you don't really know, you know, what grant is going to To fly, you know, what's going to be an avenue that will blossom and become more of your portfolio and, and what won't. a clinical academic, I think like others, I mean, I have a very mixed portfolio of funding, you know, some are sort of, you know, charities, some as UKRIs, some industry. So I think knowing, you know, Because the temptation is just to say yes to everything and just go because you don't know and then it's kind of feast or famine, so, you know, so I think that is probably the biggest challenge. And again, I don't claim to have a good answer for that.
Sandrine:So the, the podcast where our conversation will be posted is called research lives and cultures. How do you think your contributes to the research culture in a positive way? What are the, I don't know, the practices, the the rituals, how are you trying to influence through your action and maybe through pushing certain agendas. What's your role when you think about research culture?
Thushan:So you mentioned committees, there's two, I guess, formal roles that I think, you know, hopefully I contribute. One is I'm on the Wellcome Trust early career award interview committee, something I enjoy hugely and I must say my kind of non clinical, non research work, that's probably the thing that I enjoy the most. It's kind of seeing the new exciting science and trying to kind of You know help that process of selecting the, the, the next leaders research. And the second is you know, not, not too long ago became scientific secretary for the British Infection Association. So again, there's a role there of trying to kind of, you know, help with grant administration and selection and awards hope that mentorship is one of them. I mean, it's something that I see so Done so poorly, unfortunately, in, in many cases and I think it just takes a lot of efforts and a lot of application to try and mentor early career researchers properly. So, you know, again, you know, I, I'm also learning, but it's something that I hope I'm starting to do well and allow others to kind of develop. I think from a. Group perspective increasingly I'm not the one who knows the most about a topic. Right. And so I think hopefully having a sort of non hierarchical kind of structure to that and encouraging people to help each other. Because there are experts within the group who's not me So, I mean, that's all kind of research based. There's obviously, I mean, I think research culture is a very ill defined you know, topic, and it means different things to different people, but I think that's absolutely fine, right? And I think we need to be more open about the fact that it shouldn't be a rigid thing. It isn't just about EDI, you know, it isn't just about this X, Y, Z but encourage people to develop a personal strategy for what, you know, a, a better research culture means.
Sandrine:So if you were going to, do all this career all over again, what advice would you give to your young self?
Thushan:I, I think clearly picking the right mentors, I mean, it's a recurring topic, isn't it? Is, is important. I think, you know, I, I, you know I hope I, I've done that. I think I have done that. Maybe the things that would have changed probably thinking a bit more about specific skills development during my PhD. I thought I thought more about it during career development stage, but, you know you realize. Both from a clinical and a academic sense that once you become more senior that really the opportunities for really learning new skills become less and less. And partly because you're spread quite thinly and you can't spend a whole month learning a new technique. But partly because there are others who do it better. But so I think I probably would have you know, thought a bit more carefully about what specific skills in terms of, you know, analytical skills that I, I would, you know, spend more time getting formal training. I think that's probably the key thing.
Sandrine:So have more tools in your toolbox.
Thushan:I think so. I mean, you know, some, I was lucky to kind of, be trained in quite a lot of laboratory techniques during my PhD that, you know. I actually have now come right through to some of our research projects now. I think you know, the, the sort of data analytics have become more and more important over the last you know, decade, I think, you know, maybe there was less emphasis on it when I was doing my PhD, but I try to go on training courses for them, but never with the expectation that I will become an expert because I really don't have the time to do that. But more so I can have informed and intelligent conversations with the people who are experts about it. Yeah.
Sandrine:So is there a question that I haven't asked and that you, you feel I should have asked?
Thushan:I mean, I think we've touched on all of this, but just to re emphasize, I think protected time is important, right? Whether early, mid, or, you know, later career stage. I think one of the days as a clinical academic where you can do research on the side, you know, the NHS is busy, your job plans are full. So, I think we have to create space for people to be, become academics. There are many deficiencies in the path to become clinical academics, but one thing that UK has done well is to have this dual training path. There are opportunities at each clinical stage to have some protected time, but there needs to be more of them. I'm Not saying it's perfect, but I think that's important. Protective time is important and finding the right mentor. I mean, again, especially in the run up to fellowship applications it, you know, someone that will really have that iterative process with you to develop your application, you know, tell you how important it is to have, you know, three, four mock interviews and really just, just, just guide you through that process to prepare you. So you can deliver the best you can, I think is really key. And it's just very sad that that doesn't happen, you know, as often as it should.
Sandrine:So the, the last question that I have for you is about joy. The joy is not a term that we often use, but it's, what gives you joy in research.
Thushan:So learning new things, I think but I was reflecting on this thinking about your questions that actually it's the thing that attracted me to the speciality I do as well. You know, infectious diseases is, it's a non organ based, it's a very broad speciality. There's, you know, lots of unknowns when you see patients and see what they, so learning new things and, you know, not doing the same thing over and over again. Yeah. Absolutely. I've realized is something that gives me joy. So both in the clinical sphere and, and the research sphere and, and discovery, which kind of goes along with that, I think. And finally, if I may, you know, it's working with nice people. I think, I think I can't emphasize that more. It really, you know, it may sound like a very simple thing to say, but you know, yeah, working with nice people and doing exciting sort of science together is, is really what brings me joy.
Sandrine:And I couldn't, you know, emphasize that more, but I will agree with you. Yeah. Working with nice people and and creating the space for people to, to flourish,
Thushan:Absolutely.
Sandrine:It's been a pleasure. Thank you so, so much for taking the time to have this conversation with me. Much, much appreciated.
Thushan:No problem. Thanks for the invite again.
Sandrine:Thank you.